You’re Not Failing at Hypothyroidism — You Were Just Taught It Wrong
By Kai Turner
For many people, the early months after a hypothyroidism diagnosis feel less like relief — and more like confusion.
If you were recently diagnosed with hypothyroidism and feel more confused than relieved, you’re not imagining things.
You do the “right” thing.
You take the medication.
You expect energy to return.
You expect weight to normalize.
And instead?
You gain weight.
You feel slower.
Your body feels unfamiliar.
And nothing seems to line up with what you were told.
This is the part no one prepares you for.
The Diagnosis That Was Supposed to Fix Everything
When I was diagnosed with hypothyroidism, I thought clarity was finally coming.
There was a label now.
A reason for the fatigue.
A reason for the weight gain.
A plan.
Start medication → body improves → life moves forward.
That’s the story most of us are told.
What actually happened was the opposite.
I Gained Weight for Almost a Year After Starting Treatment
Within months of starting thyroid medication, I gained weight.
Not rapidly.
Not dramatically.
But steadily — and stubbornly.
This was confusing on a deep level.
My labs were improving.
My TSH was coming down.
Doctors told me things were “working.”
Yet my body felt heavier.
Slower.
More resistant.
That disconnect is brutal — especially when you’re doing everything you’re told.
And this is where many people quit, panic, or start blaming themselves.
When Weight Gain Is a Sign of Coming Out of Survival Mode
Another piece of this puzzle has nothing to do with calories, willpower, or even metabolism.
It has to do with safety.
Before treatment, my body wasn’t just hypothyroid — it was in survival mode. I was running on stress chemistry just to function. I felt an almost compulsive need to stay in motion: long walks, constant movement, always “doing something.” If I stopped, I would crash. My system only knew two gears: overdrive or shutdown.
As thyroid function stabilized, that emergency fuel supply began to turn off. For the first time in a long while, my nervous system didn’t need to stay activated just to keep me upright. Rest became possible. Stillness felt safer. And with that shift, energy output naturally dropped.
Some weight gain during this phase isn’t failure — it’s the body finally leaving alarm mode.
It Wasn’t Just Adrenaline
Adrenaline was part of it, but it wasn’t the whole story. Several systems had been compensating for low thyroid function and chronic stress at the same time:
Cortisol: the long-term stress hormone that helps maintain blood sugar and energy when metabolism is inefficient
Sympathetic nervous system: the fight-or-flight state that keeps muscles primed, mind alert, and movement constant
Cellular energy pathways: emergency modes that burn fuel quickly instead of efficiently
Dopamine drive: the chemical push that creates restlessness, urgency, and the feeling that stopping is unsafe
When thyroid signaling improved, these systems didn’t need to carry the load anymore. The chemical “push” faded. The body stopped burning energy just to stay functional.
Why the Body Slows Before It Heals
This transition can feel unsettling:
Less nervous energy
Less compulsive movement
More need for rest
A quieter internal drive
But this isn’t decline — it’s regulation.
A system that was once forced to run on stress is learning how to operate on normal metabolic rhythm again. Weight changes during this phase don’t mean something is wrong.
They often mean the body finally feels safe enough to stop running.
The Part No One Talks About: The Adjustment Curve
Here’s the truth that should be said upfront:
Treating hypothyroidism isn’t a switch — it’s a recalibration.
Your body doesn’t instantly trust the new hormonal environment.
It doesn’t immediately release stored weight.
It doesn’t suddenly behave like it did before thyroid dysfunction.
For many people, there is an adjustment curve:
Metabolism shifts slowly
Appetite signals change
Fluid balance fluctuates
Stress hormones adapt
Nutrient demands increase
Weight gain during this phase isn’t failure — it’s a system re-learning balance.
But that’s only part of the story.
The Overlooked Layer: Vitamin and Mineral Deficiencies
What really extended my confusion was something I didn’t even know to look for.
Despite improving thyroid labs, I still felt off.
Fatigue lingered.
Progress stalled.
So I pushed for deeper blood work.
That’s when I found out I was low in ferritin — and low in iodine.
And this changed everything.
Ferritin: The Missing Link for Many Thyroid Patients
Ferritin is your body’s stored iron.
Not just iron floating in the blood — but the reserve your body actually uses.
Here’s why this matters so much with hypothyroidism:
Iron is required for proper thyroid hormone production
Iron is needed for converting T4 into active T3
Low ferritin can mimic or worsen hypothyroid symptoms
Thyroid medication can increase iron demand
So you can have:
“Normal” iron levels
“Improving” thyroid labs
And still feel exhausted, heavy, and stalled
If ferritin is low.
This is incredibly common — and incredibly overlooked.
Once I saw my ferritin was low, a lot of things suddenly made sense.
Iodine: Another Piece People Are Afraid to Mention
Iodine is essential for thyroid hormone production — yet it’s often avoided or ignored entirely.
In my case, testing revealed iodine levels below optimal.
Not extreme.
Not dramatic.
But enough to matter.
Without sufficient iodine:
Thyroid hormone synthesis struggles
Medication may not feel as effective
The system remains inefficient
Correcting this wasn’t about megadoses or extremes — it was about restoring adequacy.
Why These Labs Aren’t Always Ordered — And How to Talk to Your Doctor About Them
It’s also worth understanding why many doctors hesitate to order ferritin or iodine labs in the first place.
Primary care physicians are trained to follow broad clinical guidelines. These usually focus on TSH and basic thyroid panels, not nutrient status, unless there’s a clear red flag like anemia or a severe deficiency.
Time constraints, insurance limitations, and concerns about over-supplementation can also play a role.
That doesn’t mean your concerns aren’t valid. It simply means you may need to advocate calmly and specifically.
Bringing up ongoing symptoms, asking how nutrient levels interact with thyroid function, and requesting labs as a way to rule things out — not self-diagnose — can help move the conversation forward.
And if progress continues to stall, this is where seeing an endocrinologist can be helpful. A specialist is often more comfortable looking at the full thyroid ecosystem — hormones, cofactors, and long-term trends — while still coordinating care with your primary doctor rather than working against them.
Other nutrients commonly discussed in thyroid health (even if levels are normal for many people) include:
Vitamin D — supports immune balance and is frequently low in people with autoimmune thyroid conditions
Vitamin B12 — important for energy, nerve function, and red blood cell health; deficiency can mimic hypothyroid fatigue
Selenium — involved in thyroid hormone conversion and antioxidant protection of the thyroid gland
Zinc — plays a role in hormone signaling, metabolism, and appetite regulation
Magnesium — supports stress response, muscle function, and overall metabolic calm
Not everyone with hypothyroidism will be low in these — I wasn’t — but they’re often part of a more complete thyroid workup when symptoms don’t match lab results.
The Turning Point: When My Body Finally Balanced Out
Here’s the part I wish someone had told me earlier:
The body catches up — but on its own timeline.
After addressing ferritin.
After correcting iodine.
After months of consistency.
After Staying consistent with exercise, managing stress and getting enough sleep
My weight stopped climbing.
My energy stabilized.
My body felt less resistant.
Not overnight.
Not dramatically.
But steadily — and sustainably.
The “failure phase” wasn’t failure at all.
It was the body recalibrating under new conditions.
Is this a lot? Yes
Do I wish I didn’t have to worry about any of this? Yes
Is it worth it for my health?
YES
Why Hypothyroidism Feels So Confusing at First
Hypothyroidism is confusing because:
Labs don’t tell the full story
Symptoms lag behind numbers
Nutrient deficiencies muddy the picture
Improvement isn’t linear
Weight changes don’t behave logically at first
And most people are never told to expect this.
So they assume they’re broken.
Or doing it wrong.
Or doomed to struggle forever.
They’re not.
If You’re Early in This Journey, Read This Carefully
If you’re newly diagnosed — or frustrated months in — here’s what matters most:
Healing isn’t instant
Weight gain during adjustment is common
Ferritin matters more than most people realize
Iodine adequacy matters too
Balance comes from patience plus precision
You’re not failing.
You’re adapting.
And once your system finds equilibrium, progress feels completely different.
Final Thought
Hypothyroidism doesn’t require perfection.
It requires understanding.
And the most dangerous thing isn’t slow progress —
it’s quitting before your body has time to respond.
If this resonated, you’re not alone.
You’re early — not broken.
And that distinction changes everything.
- Kai Turner
🌱One Small Thing That Helped During the Adjustment Phase
If you’re in this adjustment phase, one small thing that helped me was having a simple way to stay organized without obsessing.
A basic weekly pill organizer took mental weight off my plate — not to micromanage my body, but to create a little steadiness while things settled.
When your system is recalibrating, clarity and consistency matter more than perfection. And sometimes it’s the quiet, practical tools that help the most.
📝 Notes on Iron, Digestion, and Finding What Works
If you happen to be low in ferritin like I was, iron support can become part of the conversation — but it isn’t always straightforward.
Iron supplements can be tricky for digestion. Side effects like constipation or stomach discomfort are a common reason people struggle to stay consistent.
A lot of this comes down to form. Traditional iron supplements are often harsher on the gut, while chelated forms like iron bisglycinate are commonly better tolerated because they’re bound to an amino acid and tend to be gentler on digestion.
Hydration, adequate fiber, and thoughtful timing can also influence how well iron is tolerated, which is why digestion matters as much as the lab numbers.
For me, getting iron from food when possible felt even easier — and more enjoyable. Ordering stuffed clams at a favorite seafood spot, with crispy panko and a touch of chorizo, became an occasional treat that also happens to be extremely rich in iron. It made supporting ferritin feel less like a chore and more like a normal, sustainable part of life.
I’m Kai Turner.
I write about thyroid health, metabolism, and sustainable progress, with an emphasis on long-term balance rather than quick fixes or fear-based advice.


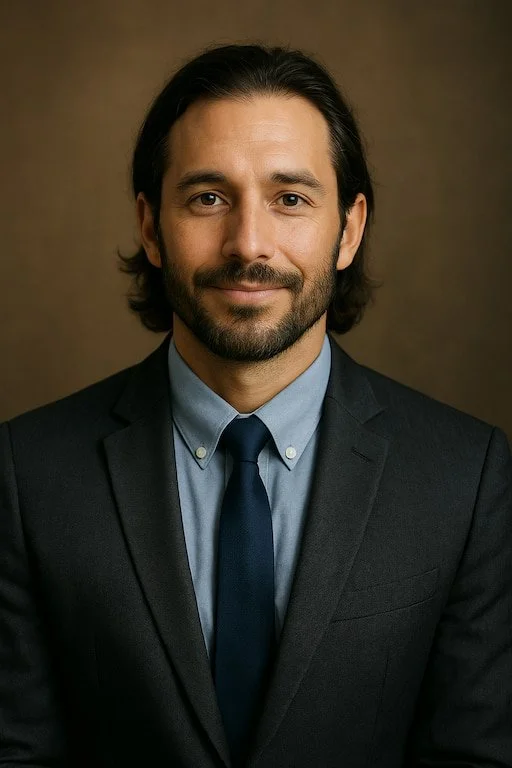













By Kai turner